Chapter Nineteen, Part 1: Metabolic Acidosis, The Show
This is it, the chapter we have all been waiting for, metabolic acidosis. And I just realized that I did not post the exciting conclusion to chapter 18. I’ll get to it next. My bad.
References
Chapter 19, Part 1
Metabolic acidosis June 14, 2023
American Society of Nephrology | Medical Students - Kidney TREKS this is the program that Josh mentioned at Mount Desert Island!
Effects of pH on Potassium: New Explanations for Old Observations - PMC here’s the review melanie from Peter Aronson that clarifies the fact that there are no H+-K+ antiporters outside the kidney but rather coupled transport-
We discussed whether we like “Winter’s formula” Quantitative Displacement of Acid-Base Equilibrium in Metabolic Acidosis | Annals of Internal Medicine
Dr. R. W. Winters was charged with larceny https://www.nytimes.com/1982/05/16/nyregion/ex-columbia-u-doctor-charged-with-larceny.html
JCI - The Maladaptive Renal Response to Secondary Hypocapnia during Chronic HCl Acidosis in the Dog this was a classic experiment exploring the respiratory response to an infusion of HCl but the animals were maintained in a high pCO2 milieu (not generalizable to humans!)
Here’s the thoughtful Pulmcrit post (by Josh Farkas) that Josh mentioned regarding correction of anion gap for hypoalbuminemia: Mythbusting: Correcting the anion gap for albumin is not helpful
JC mentioned that the anion gap does change in cirrhosis when the albumin is very low but using the correction factor may not change the clinical findings Acid-base disturbance in patients with cirrhosis: relation to hemodynamic dysfunction
Diagnostic Importance of an Increased Serum Anion Gap | NEJM Melanie mentioned the work of Patricia Gabow on the anion gap. In this review, she refers to work that she had done to try to identify all the organic anions in the anion gap but it falls short.
Also, check out this critical look at the delta/delta: The Δ Anion Gap/Δ Bicarbonate Ratio in Lactic Acidosis: Time for a New Baseline?
Roger mentioned near drowning in the Dead Sea and the unusual electrolytes in that instance. Near-Drowning in the Dead Sea: A Retrospective Observational Analysis of 69 Patients
We discussed this classic NEJM article by Daniel Batlle The Use of the Urinary Anion Gap in the Diagnosis of Hyperchloremic Metabolic Acidosis
Amy mentioned this review from Uribarri and Oh in JASN on the urine anion gap: The Urine Anion Gap: Common Misconceptions
Joel has a great blog post on the urine osmolar gap. urine osmolar gap – Precious Bodily Fluids
Anna’s VoG on the bicarb deficit: Kurtz, I Acid-Base Case Studies, 2nd Edition. Trafford Publishing 2004. And the Fernandez paper that derived a better equation
Reference for Josh’s VoG: Key enzyme in charge of ketone reabsorption of renal tubular SMCT1 may be a new target in diabetic kidney disease
Severe anion gap acidosis associated with intravenous sodium thiosulfate administration
Sodium Thiosulfate Induced Severe Anion Gap Metabolic Acidosis
Sodium Thiosulfate and the Anion Gap in Patients Treated by Hemodialysis
Outline: Chapter 19 Metabolic Acidosis
Overview
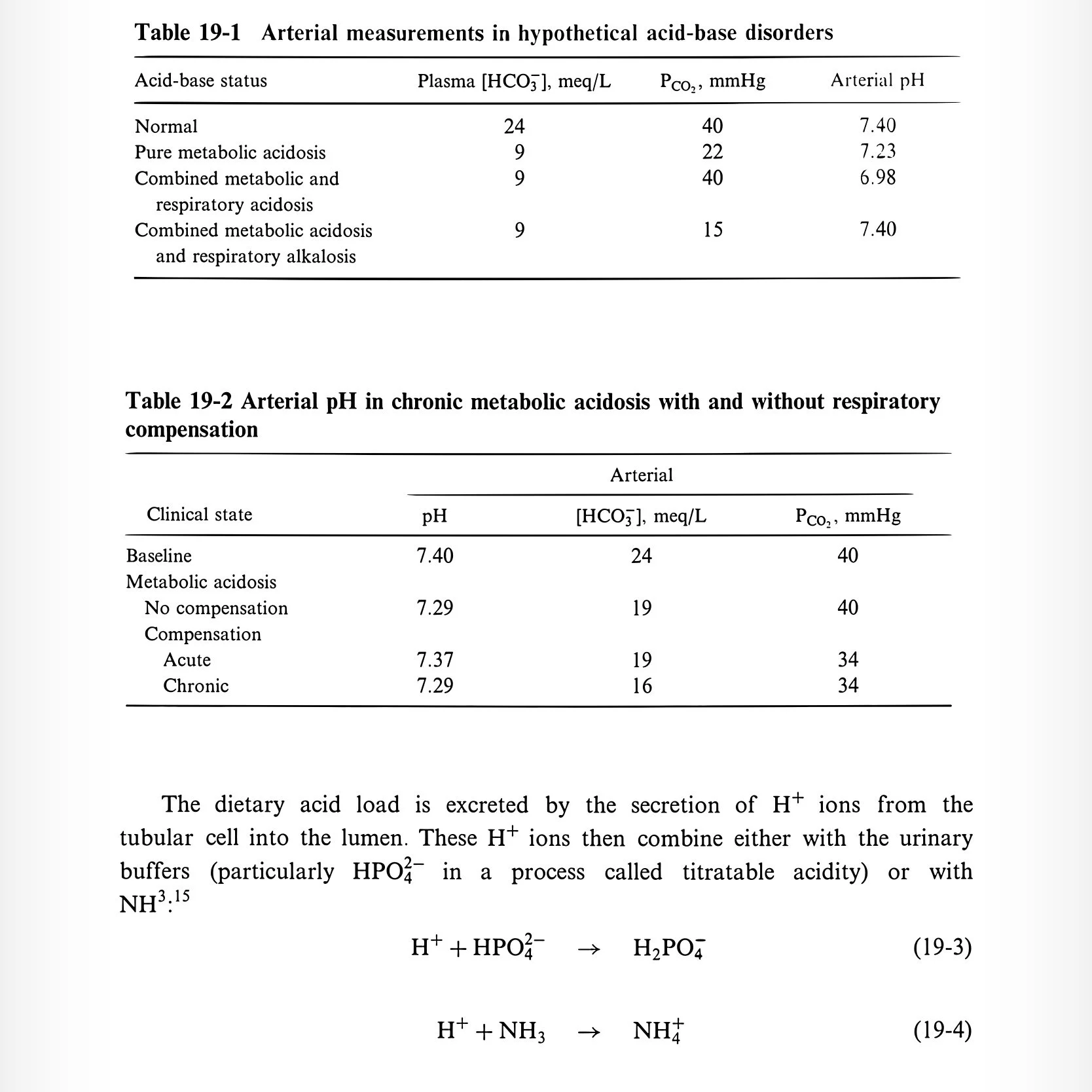
Low arterial pH
Reduced HCO3
Compensatory hyperventilation (↓ pCO2)
Bicarb < 10 strongly suggests metabolic acidosis (renal compensation for respiratory alkalosis does not go that low)
Pathophysiology
H+ + HCO3- <=> H2CO3 <=> CO2 + H2O
Acidosis results from H+ addition or HCO3 loss
Response to Acid Load
Extracellular buffering
Example: Add 12 mmol H+/L → HCO3 falls from 24 → 12 → pH drops to 7.1 (40 to 80 nmol/L)
Intracellular and bone buffering
55–60% buffered intracellularly and in bone
12 mEq/L acid load only reduces serum HCO3 by ~5 mEq/L
H+ into cells → K+ out (hyperkalemia)
Notably in diarrhea or renal failure
Less effect with organic acidosis (e.g., DKA, lactic acidosis)
Respiratory compensation
Stimulates chemoreceptors → ↑ tidal volume (more than RR)
Decreases pCO2, increases pH
Begins within 1–2 hours; peaks at 12–24 hours
Winters formula alternative: for every 1 mEq ↓ HCO3, pCO2 ↓ by 1.2
Chronic: respiratory compensation is blunted by renal adaptation
Renal hydrogen excretion
50–100 mEq/day acid generated from diet
90% filtered HCO3 reabsorbed in PT
Acid secreted:
10–40 mEq via titratable acid (TA)
30–60 mEq via NH3/NH4 (can ↑ to 250 mEq in acidosis)
TA: phosphate (DKA → ketones act as TA)
Max excretion up to 500 mEq/day in severe acidosis
Generation of Metabolic Acidosis
Mechanisms
Inability to excrete H+ (slow)
Addition of H+ or loss of HCO3 (rapid)
Anion Gap (AG)
Normal: 5–11 (falling due to rising Cl-)
Mostly due to negatively charged proteins (albumin)
Adjust for albumin: AG ↓ 2.5 per 1 g/dL albumin ↓
Revised: AG = unmeasured anions - unmeasured cations
↑ AG = addition of unmeasured anions (e.g., lactate, ketones)
Hyperchloremic acidosis: ↓ HCO3 replaced by ↑ Cl (normal AG)
Delta–Delta Analysis
Adjust AG for albumin
Normal ΔAG:ΔHCO3 = 1.6:1 (early 1:1)
<1 → high + normal AG acidosis
Other causes of AG variation
High AG without acidosis: hemoconcentration, alkalosis
Low AG: hypoalbuminemia, ↑ unmeasured cations (lithium, IgG, lab artifact)
Urine Anion Gap (UAG)
Normal = ~0; should be very negative (< -20) in acidosis
Type 1 & 4 RTA → UAG positive or near zero
Invalid in ketoacidosis or volume depletion (Na retention → ↓ distal acidification)
Urine Osmolal Gap
Estimate NH4+ via osmolar gap
Requires urine Na, K, glucose, urea
Etiologies and Diagnosis
Lactic Acidosis
Pyruvate → lactate (LDH; NADH → NAD+)
Normal production: 15–20 mmol/kg/day
Metabolized in liver/kidney → pyruvate → glucose or TCA
Normal lactate: 0.5–1.5 mmol/L; acidosis if > 4–5 mmol/L
Causes:
↑ production: hypoxia, redox imbalance, seizures, exercise
↓ utilization: shock, hepatic hypoperfusion
Malignancy, alcoholism, antiretrovirals
D-lactic acidosis
Short bowel/jejunal bypass
Glucose → D-lactate (not metabolized by LDH)
Symptoms: confusion, ataxia, slurred speech
Special assay needed
Tx: bicarb, oral antibiotics
Treatment
Underlying cause
Bicarb controversial: may worsen intracellular acidosis, overshoot alkalosis, ↑ lactate
Target pH > 7.1; prefer mixed venous pH/pCO2
Ketoacidosis (Chapter 25 elaborates)
FFA → TG, CO2, H2O, ketones (acetoacetate, BHB)
Requires:
↑ lipolysis (↓ insulin)
Hepatic preference for ketogenesis
Causes:
DKA (glucose > 400)
Fasting ketosis (mild)
Alcoholic ketoacidosis
Poor intake + EtOH → ↓ gluconeogenesis, ↑ lipolysis
Mixed acid-base (vomiting, hepatic failure, NAGMA)
Congenital organic acidemias, salicylates
Diagnosis:
AG, osmolar gap (acetone, glycerol)
Ketones: nitroprusside only detects acetone/acetoacetate
BHB can be 90% of total (false negative)
Captopril → false positive
Treatment:
Insulin +/- glucose
Renal Failure
↓ excretion of daily acid load
GFR < 40–50 → ↓ ammonium/TA excretion
Bone buffering stabilizes HCO3 at 12–20 mEq/L
Secondary hyperparathyroidism helps with phosphate buffering
Alkali therapy controversial in adults
Ingestions
Salicylates
Symptoms at >40–50 mg/dL
Early: respiratory alkalosis → Later: metabolic acidosis
Treatment: bicarb, dialysis (>80 mg/dL or coma)
Methanol
Metabolized to formic acid → retinal toxicity
Osmolar gap elevated
Tx: bicarb, ethanol/fomepizole, dialysis
Ethylene glycol
→ glycolic/oxalic acid → renal failure
Same treatment + thiamine/pyridoxine
Other
Toluene, sulfur, chlorine gas, hyperalimentation (arginine, lysine)
GI Bicarbonate Loss
Diarrhea, bile/pancreatic drainage → loss of alkaline fluids
Ureterosigmoidostomy → Cl-/HCO3- exchange in colon
Cholestyramine → Cl- for HCO3-
Renal Tubular Acidosis (RTA)
Type 1 (Distal)
↓ H+ secretion in collecting duct → urine pH > 5.3
Etiologies: Sjögren, RA, amphotericin
Features: nephrocalcinosis, stones, hypokalemia
Diagnosis: NAGMA, persistent ↑ urine pH
Treatment: alkali (1–2 mEq/kg/d adults; 4–14 kids), K+ if needed
Type 2 (Proximal)
↓ HCO3 reabsorption
Bicarb threshold reduced → self-limited
Causes: multiple myeloma, Fanconi, ifosfamide
Features: rickets/osteomalacia, no stones, pH variable
Diagnosis: NAGMA, pH < 5.3, high FE HCO3 when HCO3 loaded
Treatment: alkali (10–15 mEq/kg/d), thiazides
Type 4
Aldo deficiency/resistance → hyperkalemia + mild acidosis
K+ inhibits NH4 generation
Tx: correct K+, consider loop diuretics
Symptoms
Hyperventilation (dyspnea)
pH < 7.0–7.1 → arrhythmias, ↓ contractility
Neurologic: lethargy → coma (CSF pH driven)
Skeletal growth issues in children
Treatment Principles
No alkali needed for keto/lactic acidosis unless pH < 7.2
Bicarbonate Deficit
Deficit = HCO3 space * (desired - actual HCO3)
HCO3 space: 50–70% of body weight
Watch for:
K+ shifts: beware hypokalemia when correcting acidosis
Na+ load in CHF
Dialysis if necessary